Accueil / Information / Aller plus loin... / Aliments / Origine animale / Les oeufs
Les oeufs
vendredi 27 mars 2009, par
L’allergie à l’œuf de poule est la cause la plus fréquente d’allergie alimentaire chez l’enfant : 28,7% des cas avant l’âge de 15 ans dans les statistiques du CICBAA. Son aspect transitoire est une autre caractéristique de cette allergie, laquelle passe au 7ème rang après 15 ans, avec seulement 3,1% des cas pour le CICBAA (comm. pers. DA Moneret-Vautrin, mai 2007).
Le Réseau d’Allergo-Vigilance avait relevé 15 observations de réactions sévères avec l’œuf (poule 14, oie 1) sur un total de 900 déclarations (mai 2010), ce qui est modeste eu égard à la présence très large de l’œuf dans l’alimentation et comparativement à l’arachide, par exemple (111 cas). De même, la survenue d’une anaphylaxie alimentaire liée à l’exercice semble très rare avec l’œuf ![]() .
.
La dynamique particulière de la réactivité à l’œuf ne se limite pas à la phase de tolérance : de nombreuses séries ont montré qu’une réactivité (au moins sérologique) pouvait apparaître chez le nourrisson avant tout contact alimentaire connu avec l’œuf. Cette sensibilisation marque une susceptibilité individuelle mais pourrait être déclenchée par le passage de protéines d’œuf dans le lait maternel (cf. ![]() ).
).
Le lien entre réactivité à l’œuf et atopie est par ailleurs retrouvé dans les résultats de plusieurs travaux prospectifs : une positivité pour l’œuf dans la première année de vie est associée à un risque accru de sensibilisation respiratoire et d’asthme dans les années qui suivent ![]() .
.
L’étude longitudinale menée par Hattevig pourrait résumer ces aspects dynamiques ![]() : avec un test in vitro détectant des niveaux très bas d’IgE-réactivité, des profils différents sont vus selon les enfants :
: avec un test in vitro détectant des niveaux très bas d’IgE-réactivité, des profils différents sont vus selon les enfants :
- certains présentent une réactivité transitoire, tant pour l’œuf que pour le chat ou les acariens, et seront classés plus tard comme « non atopiques »
- d’autres voient leur réactivité initiale se maintenir ou tarder à se corriger et conservent leur tendance « atopique » avec l’âge.
L’allergie à l’œuf associée à une sensibilisation respiratoire aux oiseaux
Cette entité a été nommée le syndrome « œuf – oiseaux » et est abordée dans le thème des oiseaux.
Allergie respiratoire à l’œuf
Une expression clinique volontiers respiratoire est notée avec l’œuf chez les patients avec syndrome œuf-oiseaux.
Dans un cadre d’exposition professionnelle, on peut assister à une sensibilisation respiratoire à l’œuf (ex. métiers de la confiserie, fabrication d’œuf en poudre, etc..).
Celle-ci s’accompagne-t-elle d’une allergie alimentaire à l’œuf ? La littérature est pauvre sur ce sujet et rares sont les cas publiés d’allergie initialement respiratoire se compliquant par la suite d’une allergie alimentaire pour l’œuf ![]()
![]() .
.
Le lysozyme d’œuf peut lui-même entraîner un asthme professionnel ![]() .
.
Allergie alimentaire à d’autres œufs que l’œuf de poule
En général, on assiste à une réactivité aux œufs d’autres oiseaux chez les patients allergiques à l’œuf de poule ![]()
![]() . Cette réactivité croisée est rencontrée également dans le syndrome œuf-oiseaux.
. Cette réactivité croisée est rencontrée également dans le syndrome œuf-oiseaux.
Cependant, quelques cas d’allergie à l’œuf de caille sans allergie (ni TC ou CAP positifs) pour l’œuf de poule ont été rapportés, tant chez l’adulte que chez l’enfant ![]()
![]() . La négativité en blot s’étendait aussi au canard et à l’oie. Les allergènes en cause n’ont pas été identifiés.
. La négativité en blot s’étendait aussi au canard et à l’oie. Les allergènes en cause n’ont pas été identifiés.
Les allergènes de l’œuf
Blanc d’œuf
Une analyse protéomique a permis récemment d’agrandir la liste des molécules IgE-réactives du blanc d’œuf ![]() : on en dénombre ainsi pas moins de 20. Toutes n’ont pas un statut allergénique sûr
: on en dénombre ainsi pas moins de 20. Toutes n’ont pas un statut allergénique sûr ![]() .
.
Certaines protéines sont plus difficiles à détecter du fait de leur masse (ovomucine 8000 kD, ovostatine 780 kD). Les ovomucines sont responsables du pseudo-gel du blanc d’œuf à l’état natif.
Le tableau ci-dessous liste les protéines par ordre décroissant de concentration dans le blanc d’œuf ![]() :
:
| % des protéines | Nom commun | Nom IUIS | Fonction | Masse |
|---|---|---|---|---|
| 54 | Ovalbumine | Gal d 2 | Serpine | 44 et+ |
| 12 | Ovotransferrine (= conalbumine) |
Gal d 3 | Transferrine | 78 |
| 11 | Ovomucoïde | Gal d 1 | Inhibiteur de type Kazal | 28 |
| 8 ? | G2 et G3 globulines | |||
| 3,5 | Ovomucine | 8000 | ||
| 3,4 | Lysozyme | Gal d 4 | Hydrolase | 14 |
| 1,5 | Ovoinhibiteur | Inhibiteur de type Kazal | 63-69 | |
| 1 | Ovoglycoprotéine | Lipocaline | 37-42 | |
| 0,5 | Ovostatine | 780 | ||
| 0,05 | Cystatine | 11 | ||
| 0,05 | Avidine | 60 |
- l’ovomucoïde, Gal d 1, est la protéine dominante pour l’allergénicité du blanc d’œuf

- l’ovalbumine, Gal d 2, se présente sous des formes plus ou moins glycosylées et phosphorylées et peut aussi se polymériser
 . C’est un inhibiteur de sérine protéase appartenant à la famille des serpines
. C’est un inhibiteur de sérine protéase appartenant à la famille des serpines  .
. - le lysozyme, Gal d 4, est une glycosyl-hydrolase à activité muramidase et chitinase. Il est fréquemment utilisé en industrie agro-alimentaire (ex. fromages). Il ne croise pas avec le lysozyme humain
 ni avec l’alpha-lactalbumine du lait de vache
ni avec l’alpha-lactalbumine du lait de vache  .
.
Le lysozyme peut être la cause d’une allergie médicamenteuse, avec allergie à l’œuf déjà connue , ou même avant tout contact avec l’œuf
, ou même avant tout contact avec l’œuf 
- l’avidine possède une affinité de liaison extrêmement élevée avec la biotine. D’où un effet anti-microbien dans la blanc d’œuf
 . Une IgE-réactivité a été suggérée pour cette protéine
. Une IgE-réactivité a été suggérée pour cette protéine  , mais reste à prouver. Certaines techniques in vitro utilisent des allergènes biotinylés et l’équivalent bactérien de l’avidine, la streptavidine. Mais cela n’entraîne pas, a priori, d’interférence dans les tests d’IgE-réactivité pour le blanc d’œuf.
, mais reste à prouver. Certaines techniques in vitro utilisent des allergènes biotinylés et l’équivalent bactérien de l’avidine, la streptavidine. Mais cela n’entraîne pas, a priori, d’interférence dans les tests d’IgE-réactivité pour le blanc d’œuf. - on trouve aussi une protéine liant la riboflavine, une clustérine, une ovalbumine Y
 , etc…
, etc…
Les prévalences de positivité pour les allergènes du blanc d’œuf sont à peu près équivalentes entre ovalbumine, ovomucoïde et ovotransferrine. Ces 3 allergènes sont en général positifs ensemble chez 60 à 80% des patients allergiques à l’œuf. Le lysozyme est moins souvent positif ![]() mais son importance est peut-être sous-estimée
mais son importance est peut-être sous-estimée ![]() .
.
Il faut souligner un autre point important au sujet des allergènes du blanc d’œuf : beaucoup de travaux ont utilisé des protéines d’œuf d’origine commerciale (ex. Sigma). Ces produits ne sont pas 100% purs. Par exemple, l’ovalbumine est contaminée par de l’ovomucoïde ![]()
![]() , ou ce dernier par du lysozyme
, ou ce dernier par du lysozyme ![]() . Cela n’est pas sans incidence sur les résultats de certains travaux.
. Cela n’est pas sans incidence sur les résultats de certains travaux.
Les protéines du jaune d’œuf sont de 3 sortes :
- des lipoprotéines de basse densité (LDL) qui représentent environ 60 % des protéines. D’origine hépatique, elles sont clivées dans le jaune avec formation d’apovitellenines
 . Ces protéines sont IgE réactives.
. Ces protéines sont IgE réactives. - des protéines associées en granules et dérivant d’un précurseur hépatique, la vitellogénine : on distingue la lipovitaline (à priori non allergisante) et la phosvitine (IgE-réactive). Cette dernière a un rôle important de chélation du fer.
- des livétines qui se présentent sous des formes variées allant de 45 à 150 kD et sont équivalentes à l’albumine (alpha livétine = Gal d 5), à l’alpha-2 macroglobuline (béta livétine) et aux γ globulines (gamma livétines) trouvées dans le sérum des oiseaux.. Ces livétines sont le support des réactions croisées du syndrome œuf-oiseaux (cf. Albumines).
Œufs : stabilité à la chaleur et à la digestion
Parmi les allergènes d’œuf, ce sont avant tout l’ovalbumine et l’ovomucoïde qui ont été étudiés.
Des discordances entre les résultats de ces études pourraient provenir de la contamination des produits utilisés.
Résistance à la chaleur
La cuisson permet à une proportion non négligeable d’enfants de tolérer l’œuf ![]()
![]() . La cuisson doit cependant être complète sinon des réactions cliniques peuvent subsister
. La cuisson doit cependant être complète sinon des réactions cliniques peuvent subsister ![]()
![]() .
.
La majeure partie de l’allergénicité étant située dans le blanc d’œuf, la coagulation due à la chaleur peut-elle expliquer la meilleure tolérance de l’œuf cuit ? On peut supposer que la chaleur entraîne une modification des épitopes et/ou un changement des points de protéolyse au moment de la digestion :
- l’ovalbumine voit son IgE-réactivité très affectée par la cuisson (- 90 % après 3 min à 100°C
 ). L’ovalbumine donne des agrégats sitôt chauffée
). L’ovalbumine donne des agrégats sitôt chauffée  et, chez la souris, le passage d’ovalbumine dans le sang portal est aboli (15 min à 100°C
et, chez la souris, le passage d’ovalbumine dans le sang portal est aboli (15 min à 100°C  ).
). - cependant, le coagulum d’ovalbumine retient des solutés : il faut un lavage intense du blanc d’œuf cuit pour que le pouvoir allergisant chez la souris soit annulé
 . Cela a été retrouvé aussi en TPO par Urisu
. Cela a été retrouvé aussi en TPO par Urisu  .
. - d’autres allergènes résistent mieux à la chaleur
 : le lysozyme, la conalbumine et surtout l’ovomucoïde
: le lysozyme, la conalbumine et surtout l’ovomucoïde  . Et ce dernier est plus souvent positif chez les enfants non tolérants à l’œuf même cuit
. Et ce dernier est plus souvent positif chez les enfants non tolérants à l’œuf même cuit 
- si la digestibilité de l’ovomucoïde n’est pas changée par la cuisson
 , les conditions expérimentales ne traduisent pas toujours la réalité clinique. Les autres ingrédients de l’aliment peuvent jouer un rôle, tant au niveau de la digestibilité que sur l’effet de la chaleur. Kato a noté que l’ovomucoïde cuit en présence de farine de blé (mais pas de caséine) avait une IgE-réactivité abaissée
, les conditions expérimentales ne traduisent pas toujours la réalité clinique. Les autres ingrédients de l’aliment peuvent jouer un rôle, tant au niveau de la digestibilité que sur l’effet de la chaleur. Kato a noté que l’ovomucoïde cuit en présence de farine de blé (mais pas de caséine) avait une IgE-réactivité abaissée  . Dans d’autres études il a été observé que la cuisson diminuait l’IgE-réactivité des protéines d’œuf dans des gâteaux ou des pâtes, mais pas dans des produits sans farine (viande hachée, mayonnaise, etc..)
. Dans d’autres études il a été observé que la cuisson diminuait l’IgE-réactivité des protéines d’œuf dans des gâteaux ou des pâtes, mais pas dans des produits sans farine (viande hachée, mayonnaise, etc..) 

- la chaleur, mais aussi le stockage, conduit à une transformation de la structure III de l’ovalbumine : la S-ovalbumine qui se forme peu à peu s’avère plus stable que l’ovalbumine initiale. Le stockage, y compris à +4°C, modifie un peu les contenus mesurables d’ovomucoïde (moins 40% environ en 6 semaines) ou en lysozyme (moins 25%). Cela ne rend pas pour autant les œufs anallergiques !
- enfin, peu de travaux ont concerné les allergènes du jaune d’œuf : Quirce trouve une diminution de l’IgE-réactivité de la livétine après chauffage à 90°C
 .
.
A noter que l’ovomucoïde reste soluble (et donc extractible) après cuisson du blanc d’œuf. Cela pourrait avoir influencé le rôle important attribué à cet allergène comparativement à l’ovalbumine. Cependant, sur 17 enfants avec TPO positif pour l’œuf cuit, un seul a encore un TPO positif après élimination de l’ovomucoïde de l’œuf cuit (par rinçage extensif) ![]() . L’ovomucoïde a donc bien une réelle importance clinique.
. L’ovomucoïde a donc bien une réelle importance clinique.
Résistance à la digestion
Les résultats d’Astwood ![]() sont à présent complétés par des travaux ayant montré le rôle du pH et l’importance de surveiller la persistance de fragments IgE-réactifs
sont à présent complétés par des travaux ayant montré le rôle du pH et l’importance de surveiller la persistance de fragments IgE-réactifs ![]() . Des résultats divergents ont été rapportés pour la digestibilité des protéines d’œuf :
. Des résultats divergents ont été rapportés pour la digestibilité des protéines d’œuf :
- l’ovalbumine est dégradée à 90 % en 10 min à pH 1,2 et en 30 min à pH2
 . Mais des fragments sont présents encore après 1 h de digestion
. Mais des fragments sont présents encore après 1 h de digestion 
- l’ovomucoïde est lui aussi rapidement dégradé, des fragments IgE-réactifs étant cependant retrouvés


- le lysozyme résisterait 1 h selon Fu
 , d’autres auteurs ayant trouvé une digestibilité plus facile
, d’autres auteurs ayant trouvé une digestibilité plus facile 
La cuisson augmente la digestibilité de l’ovalbumine, mais pas celle de l’ovomucoïde ![]() .
.
Œufs : effets de processus techno-alimentaires
Fiocchi a montré une IgE-réactivité augmentée avec le blanc d’œuf lyophilisé ![]() . L’irradiation gamma diminuerait l’allergénicité de l’ovalbumine
. L’irradiation gamma diminuerait l’allergénicité de l’ovalbumine ![]() et celle de l’ovomucoïde
et celle de l’ovomucoïde ![]() . Les hautes pressions n’annulent pas l’IgE-réactivité de l’ovalbumine
. Les hautes pressions n’annulent pas l’IgE-réactivité de l’ovalbumine ![]() . La combinaison d’étapes de chauffage et d’hydrolyse enzymatique parviendrait à abaisser d’un facteur 100 l’IgE-réactivité du blanc d’œuf
. La combinaison d’étapes de chauffage et d’hydrolyse enzymatique parviendrait à abaisser d’un facteur 100 l’IgE-réactivité du blanc d’œuf ![]() .
.
Œufs : allergènes cachés
L’œuf et ses composants (par exemple le lysozyme) sont largement utilisés dans l’industrie agro-alimentaire.
L’ovalbumine est parfois la cause de réactions allergiques inattendues (bonbons) ![]() .
.
L’œuf arrive juste après le lait de vache comme cause d’alerte par la FAAN aux USA : 26,7 % des déclarations par les industriels de la présence par erreur d’un ingrédient allergisant dans un aliment manufacturé (n = 495 déclarations de novembre 2001 à juin 2007).
Le blanc d’œuf est utilisé comme agent d’affinage pour clarifier les vins rouges (< 10 g/hl). On peut retrouver des traces de blanc d’œuf et/ou de lysozyme dans certains vins ![]()
![]() , mais cela reste sans incidence clinique (TPODA négatif chez des patients allergiques à l’œuf
, mais cela reste sans incidence clinique (TPODA négatif chez des patients allergiques à l’œuf ![]()
![]() ).
).
Diagnostic d’une allergie à l’œuf
Diagnostic à l’aide de seuils décisionnels
La fréquence de l’allergie à l’œuf chez l’enfant, et même chez le très jeune enfant, a suscité la recherche de critères diagnostiques suffisants pour éviter d’avoir à pratiquer un TPO.
Des cohortes d’enfants ont été étudiées pour établir des seuils décisionnels, tant en TC qu’avec des tests in vitro. Ces seuils devaient avoir une valeur prédictive suffisante : celle-ci est estimée devoir atteindre au moins 95% ![]() , voire 99%
, voire 99% ![]() .
.
Tests cutanés
Prick-tests
Un seuil TC à 3 mm donne une VPP insuffisante (85-93% ![]()
![]() ). Il est généralement retenu 5 mm avant 2 ans et 7 mm par la suite
). Il est généralement retenu 5 mm avant 2 ans et 7 mm par la suite ![]()
![]()
![]() .
.
Cependant des seuils nettement plus élevés ont été proposés (ex. 13 mm pour une VPP à 95%) ainsi que d’utiliser le rapport mm œuf/mm histamine (ex. seuil à 2,6 pour VPP95%) ![]() .
.
De fait, le likehood ratio (LR), qui est un indice plus sûr que la VPP, reste peu discriminant avec des TC de l’ordre de 6 mm : LR = 2,6 ![]() ou 6,1
ou 6,1 ![]() .
.
Il a été proposé d’utiliser l’ovomucoïde en tests cutanés pour améliorer l’efficacité diagnostique : Dieguez obtient ainsi un LR à 20,4 ![]() .
.
Patch-tests
Comparativement aux prick-tests et/ou aux tests in vitro, l’efficacité diagnostique est parfois légèrement meilleure ![]() , parfois non
, parfois non ![]() . La combinaison patch + prick et/ou CAP apporte un gain modeste : par exemple 89% d’efficacité diagnostique contre 80% pour le CAP seul
. La combinaison patch + prick et/ou CAP apporte un gain modeste : par exemple 89% d’efficacité diagnostique contre 80% pour le CAP seul ![]() .
.
Tests in vitro
Le tableau ci-dessous présente les résultats des études ayant déterminé des seuils avec le CAP blanc d’œuf chez l’enfant :
Moy = moyen / Méd = médian
On peut constater une grande variabilité des seuils en kU/l d’une étude à une autre.
Peu de travaux ont été menés chez l’adulte :
| Nb sujets | Age (ans) | Prévalence (%) | Seuil (kU/l) | VPP (%) | |
|---|---|---|---|---|---|
| Norgaard 1992 |
13 | (adultes) | 54 | 0,35 17,5 |
58 60 |
| Norgaard 1995 |
15 | (adultes) | 60 | 0,35 17,5 |
69 75 |
| Ispano 1996 |
(adultes) | 0,35 | 100 |
Si des VPP d’au moins 95% étaient atteintes chez l’enfant, cela semble plus difficile chez l’adulte. Mais d’autres travaux seraient nécessaires.
Par contre, comment peut-on expliquer les disparités relevées entre les seuils chez les enfants ?
Influence du mode de recrutement
Dans la littérature, les cohortes d’enfants étudiés pour une allergie à l’œuf sont issues de populations relativement sélectionnées, particulièrement dans les services hospitaliers renommés. Ces conditions de recrutement ne sont pas représentatives d’une clientèle de ville.
Par exemple, la prévalence d’un eczéma atopique dans ces séries est tout à fait considérable : en moyenne 82% sur la base de 15 études différentes.
De même pour la prévalence d’allergie. Or, cela joue sur la valeur à accorder à un seuil décisionnel. Par exemple, pour un TC de 3 mm la VVP passe de 85% pour une proportion d’allergiques (confirmés par TPO) de 73% à 19% si cette proportion n’est que de 10% ![]() . De même pour un CAP > 7,5 kU/l : la VPP descende de 98,7% à 87,5% si la prévalence d’allergie passe de 54% à 10%
. De même pour un CAP > 7,5 kU/l : la VPP descende de 98,7% à 87,5% si la prévalence d’allergie passe de 54% à 10% ![]() .
.
L’âge des enfants composant la cohorte ayant permis de calculer le seuil décisionnel est un autre facteur essentiel à prendre en considération pour pouvoir transposer ce seuil à un autre cadre de recrutement.
Ce point a été souligné de longue date ![]() et confirmé par plusieurs auteurs
et confirmé par plusieurs auteurs ![]()
![]()
![]()
![]()
![]() .
.
A l’heure actuelle, même si l’on peut encore trouver des préconisations sans nuances ![]()
![]() , il n’est plus question de pouvoir transposer un seuil établi ailleurs que dans sa propre population de patients
, il n’est plus question de pouvoir transposer un seuil établi ailleurs que dans sa propre population de patients ![]()
![]()
![]()
![]() .
.
Les préconisations de seuils décisionnels sont d’ailleurs parfois curieuses : ainsi un diagnostic d’allergie à l’œuf est posé si le CAP dépasse 2 kU/l chez les enfants de moins de 2 ans et s’il dépasse 7 kU/l à partir de 2 ans ![]() . Que fait-on à 2 ans et 1 jour d’un résultat à 3 kU/l par exemple ?
. Que fait-on à 2 ans et 1 jour d’un résultat à 3 kU/l par exemple ?
Enfin, même si l’œuf est moins concerné que la farine de blé, par exemple, la survenue de réactions retardées n’est pas prise en compte dans les calculs de certains seuils. Cela ajoute à la disparité constatée entre les valeurs en kU/l pour une même probabilité d’allergie : c’est bien seulement là où les seuils ont été établis qu’ils peuvent être utiles.
Influence de l’eczéma atopique
Dans un groupe d’enfants vus pour suspicion d’allergie à l’œuf, on trouve plus d’enfants avec un eczéma atopique si le TPO pour l’œuf est positif que s’il est finalement négatif (env. 20% en plus ![]()
![]() ).
).
Des résultats > 17,5 kU/l pour le CAP blanc d’œuf sont nettement plus fréquents si l’atteinte eczémateuse est sévère (32%) plutôt que légère (3%) ![]() .
.
La réactivité à l’œuf favorise-t-elle l’eczéma ? Ou, au contraire, la pathologie sous-jacente à l’eczéma s’accompagne-t-elle d’une déviation immunologique sensibilisante ?
Le fait est que chez des enfants recrutés pour leur eczéma on a relevé de 40 à 80% de CAP blanc d’œuf positifs. Et 7% seraient déclarés allergiques à l’œuf avec les seuils Sampson ![]()
![]() .
.
Il a été suggéré que les taux très élevés d’IgE totales fréquemment rencontrés en cas d’eczéma atopique pourraient fausser les niveaux des réactivités « spécifiques ». Mais, la fréquence des résultats > 1000 UI/ml chez ces patients n’est pas très élevée (moins de 4% ![]() ). D’ailleurs, utiliser le rapport kU blanc d’œuf/IgE totales n’améliore pas la pertinence diagnostique
). D’ailleurs, utiliser le rapport kU blanc d’œuf/IgE totales n’améliore pas la pertinence diagnostique ![]() .
.
Les courbes de risque d’allergie
Le calcul qui aboutit à une valeur prédictive positive (VPP) tient compte de la sensibilité du test, de sa spécificité et de la prévalence du trait recherché (ici l’allergie) parmi la cohorte étudiée. On a donc reproché aux VPP de dépendre trop du recrutement des patients.
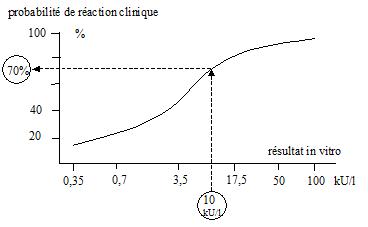
C’est pour corriger ce défaut que Sampson a introduit en 2001 un calcul probabilistique où, selon cet auteur, la prévalence ne joue pas ![]() . Le résultat de ce calcul se traduit sous la forme d’une courbe donnant un pourcentage de chances d’allergie en fonction du résultat du test (kU/l, mm, ..).
. Le résultat de ce calcul se traduit sous la forme d’une courbe donnant un pourcentage de chances d’allergie en fonction du résultat du test (kU/l, mm, ..).
Il va de soi que cette approche est séduisante. Elle a été par la suite reprise dans plusieurs travaux ![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]() . Elle a même été étendue à des courbes en 3D
. Elle a même été étendue à des courbes en 3D ![]()
![]() .
.
Les problèmes de non-transférabilité évoqués plus haut avec des seuils définis pour atteindre telle ou telle VPP restent les mêmes pour des seuils déduits de ces courbes de risque. Dans un même service hospitalier, les courbes peuvent changer d’une étude à la suivante ![]()
![]() !
!
Par ailleurs, la représentation graphique induit une illusion : celle de pouvoir donner un chiffre précis de risque d’allergie, alors qu’au moins 2 choses s’y opposent :
- la courbe n’est pas une relation unissant risque et kU/l chez un même patient, mais un ensemble de points représentant autant de patients différents : la variation dans le temps des kU/l chez un patient donné ne permet pas de déplacer le risque du patient par glissement le long de la courbe. En effet, la courbe n’est pas la moyenne des courbes individuelles des patients de la cohorte.
- de plus, l’absence quasi constante de représentation des limites de confiance (± 2 écart-types) de part et d’autre de la courbe dans les travaux publiés masque la grande imprécision des risques d’allergie qu’il s’agirait de déduire de telles courbes. par exemple :

Comme le montre le tableau ci-dessous, les courbes de risque n’ont pas résolu la question de la transférabilité des seuils.
Travaux chez l’enfant – TPO classique – Seuil CAP blanc d’œuf – Courbes de probabilité
Autres approches quantitatives
Est-ce que l’on pourrait se servir du résultat en kU/l pour chiffrer la réactivité clinique à l’œuf ?
Hélas, non : à un niveau individuel on ne peut apprécier ni la dose élicitrice ![]()
![]()
![]() , ni la sévérité des symptômes
, ni la sévérité des symptômes ![]()
![]()
![]() . Dans une série, les 5 enfants ayant eu des réactions sévères avaient même un CAP négatif
. Dans une série, les 5 enfants ayant eu des réactions sévères avaient même un CAP négatif ![]() !
!
Que peut-on tirer des valeurs extrêmement basses ?
Depuis l’alignement du seuil de positivité du CAP sur celui de l’Immulite, il est possible d’avoir des résultats chiffrés à partir de 0,10 kU/l. Cela permettait-il mieux d’exclure une allergie à l’œuf ? Il semble que non : 3,6% des cas d’allergie à l’œuf dans les données du CICBAA avaient un CAP compris entre 0,10 et 0,35 kU/l ![]() ; et dans d’autres séries ce taux s’élevait à 14%
; et dans d’autres séries ce taux s’élevait à 14% ![]() , voire 23%
, voire 23% ![]() .
.
Lemon-Mulé a avancé que l’on avait moins de 10% de TPO positifs quand le CAP ovomucoïde était < 0,1 kU/l ![]() . Cependant leurs figures montrent plutôt 20% ou plus, et ces taux ne peuvent éviter d’effectuer un TPO en pratique.
. Cependant leurs figures montrent plutôt 20% ou plus, et ces taux ne peuvent éviter d’effectuer un TPO en pratique.
Blanc d’œuf vs jaune d’œuf
Est-il utile de tester le jaune d’œuf ? Oui si l’on suspecte un syndrome œuf-oiseaux.
En revanche, dans le cas de l’allergie à l’œuf du jeune enfant, la réactivité est avant tout concentrée dans les protéines du blanc d’œuf :
- Fiocchi observe 23 TPODA positif pour le blanc d’œuf, 5 pour le blanc et le jaune d’œuf, mais aucun pour le jaune d’œuf seulement
 .
. - Takaoka relève 97 % de TPO négatifs avec le jaune d’œuf
 .
. - Et Perackis ne trouve pas de réactivité cutanée plus grande avec l’œuf entier plutôt que le blanc d’œuf
 .
.
Fiocchi retrouve en tests cutanés et en tests in vitro une mauvaise valeur prédictive positive pour le jaune d’œuf. Et, puisque les TPO avec le jaune d’œuf ne sont pas contributifs, il suggère de pratiquer les TPO de façon simple, c’est à dire avec l’œuf entier ![]() .
.
Le jaune d’œuf a fait l’objet de quelques travaux visant à déterminer des seuils diagnostiques. Les seuils obtenus pour le jaune d’œuf sont disparates, probablement pour les mêmes raisons que pour le blanc d’œuf :
Des travaux anciens sont parfois cités à l’appui d’une réactivité croisée entre blanc et jaune d’œuf ![]()
![]()
![]() . L’examen des méthodes utilisées et des résultats présentés n’est pas en faveur d’une telle conclusion.
. L’examen des méthodes utilisées et des résultats présentés n’est pas en faveur d’une telle conclusion.
La multitude des croisements relevés par Walsh ![]() , par exemple, fait plutôt suspecter la contamination des protéines testées. C’est aussi la conclusion à retirer du travail de Quirce
, par exemple, fait plutôt suspecter la contamination des protéines testées. C’est aussi la conclusion à retirer du travail de Quirce ![]() : on ne peut retenir comme significative la réactivité croisée entre blanc d’œuf et jaune d’œuf.
: on ne peut retenir comme significative la réactivité croisée entre blanc d’œuf et jaune d’œuf.
Existe-t-il un intérêt à tester certains allergènes du blanc d’œuf ?
Des résultats très disparates ont été publiés au sujet de l’importance de tel ou tel allergène de l’œuf.
Il ne semble pas y avoir de profil d’allergènes correspondant à une signification clinique particulière (signes cliniques, fixité de l’allergie). Il est possible que les résultats publiés aient été brouillés par la présence de contaminants dans les protéines utilisées et souvent acquises auprès de distributeurs de produits pour la chimie.
La « puce à allergènes » ISAC a été testée chez 60 enfants : les 3 allergènes de blanc d’œuf contenus sur la puce (ovomucoïde, ovalbumine, ovotransferrine) n’apportaient pas d’avantage significatif par rapport au CAP blanc d’œuf <10208>
Walsh et coll ![]() distinguent 4 groupes de réactivité différents, mais les limites entre groupes sont peu claires et l’utilisation clinique de cette classification n’est pas donnée.
distinguent 4 groupes de réactivité différents, mais les limites entre groupes sont peu claires et l’utilisation clinique de cette classification n’est pas donnée.
On peut cependant relever avec cette étude portant sur 40 enfants que les prévalences de réactivité sont très différents d’un allergène à un autre, avec pour le blanc d’œuf : ovomucoïde > ovalbumine > conalbumine>> lysozyme et ovomucine.
L’ovomucoïde (Gal d 1) pourrait s’avérer un peu plus discriminant que le CAP blanc d’œuf en suivi : en effet, Jarvinen a montré qu’environ les 2/3 des enfants non encore tolérants avaient un CAP Gal d 1 plus élevé que celui des enfants devenus tolérants ![]() . Et en testant 4 courts peptides issus de l’ovomucoïde, seuls les enfants non tolérants répondaient à au moins un de ces peptides. On peut cependant questionner ces derniers résultats car l’IgE-réactivité des enfants non tolérants pour l’ovomucoïde n’a pas été, avant les tests, au même niveau que celle des enfants tolérants.
. Et en testant 4 courts peptides issus de l’ovomucoïde, seuls les enfants non tolérants répondaient à au moins un de ces peptides. On peut cependant questionner ces derniers résultats car l’IgE-réactivité des enfants non tolérants pour l’ovomucoïde n’a pas été, avant les tests, au même niveau que celle des enfants tolérants.
De fait, dans la série d’Ando, un CAP ovomucoïde à 20 kU/l donnait une VPP de 95% pour un TPO positif avec œuf cuit, quand 62 kU/l étaient nécessaires en CAP blanc d’œuf ![]() . Mais Lemon-Mulé n’obtenait que 90% de probabilité de TPO positif œuf cuit avec un résultat à 50 kU/l pour l’ovomucoïde
. Mais Lemon-Mulé n’obtenait que 90% de probabilité de TPO positif œuf cuit avec un résultat à 50 kU/l pour l’ovomucoïde ![]() .
.
Suivi de l’allergie et pronostic de tolérance
En l’absence de réaction récente depuis 1 an, a-t-on des critères quantitatifs pour proposer un test de réintroduction de l’œuf ? :
- Perry estime qu’il faut avoir plus d’une chance sur 2 pour un TPO négatif : dans sa série d’enfants il obtient 59% de TPO négatifs parmi les enfants ayant moins de 2 kU/l

- Sampson a d’abord utilisé un seuil équivalent au ¼ du seuil diagnostique, soit 1,5 kU/l, pour envisager un TPO de réintroduction. Mais même avec moins de 0,7 kU/l les chances d’un TPO négatif n’étaient que de 38%
 . Aussi, une combinaison associant CAP < 2,5 kU/l et TC < 3 mm est plus efficace et permet d’espérer plus d’une chance sur 2 pour un TPO négatif
. Aussi, une combinaison associant CAP < 2,5 kU/l et TC < 3 mm est plus efficace et permet d’espérer plus d’une chance sur 2 pour un TPO négatif 
- des courbes 3D ont été construites pour tenter de déterminer une relation entre évolution des kU/l, durée de suivi et acquisition de tolérance
 . Ces courbes, qui ne sont significatives que pour les enfants diagnostiqués avant l’âge de 4 ans, sont dépourvues d’intérêt en pratique clinique : en dehors de la question de leur transférabilité à d’autres recrutements, une chute des kU/l de moitié sur 1 an offre 52% de chances de tolérance contre 40% en l’absence de modification du CAP. On a même 16% de chances de tolérance avec des valeurs ayant triplé in vitro si l’on en croît les courbes présentées !
. Ces courbes, qui ne sont significatives que pour les enfants diagnostiqués avant l’âge de 4 ans, sont dépourvues d’intérêt en pratique clinique : en dehors de la question de leur transférabilité à d’autres recrutements, une chute des kU/l de moitié sur 1 an offre 52% de chances de tolérance contre 40% en l’absence de modification du CAP. On a même 16% de chances de tolérance avec des valeurs ayant triplé in vitro si l’on en croît les courbes présentées !
Le recouvrement entre les valeurs quantitatives ne distingue donc pas clairement les patients encore allergiques de ceux qui ont acquis une tolérance à l’œuf. La pratique d’un TPO reste indispensable pour préciser la signification d’une évolution favorable des prick-tests et/ou des CAP en suivi ![]()
![]()
![]() .
.
Récemment, certains auteurs ont étudié des seuils qui permettraient d’alléger l’éviction en réintroduisant l’œuf à condition qu’il soit très cuit :
Travaux chez l’enfant – TPO avec œuf cuit – Seuil CAP blanc d’œuf
| Nb sujets | Age (ans) | Prévalence (%) | Seuil (kU/l) | VPP ou Probab. (%) | |
|---|---|---|---|---|---|
| Lemon-M. 2008 |
117 | Moy. 6,9 | 30 | 75 100 |
50 (Probab.) 65 |
| Ando 2008 |
108 | Méd. 2,8 | 35 | 4,4 62 |
68 (VPP) 95 |
D’autres travaux seraient utiles, mais il semble que ces seuils soient peu utiles en pratique car le nombre de TPO évités restera très faible (peu d’enfants avec plus de 62 ou 75 kU/l).
Cela est le cas aussi pour d’autres critères étudiés par Lemon-Mulé ![]() :
:
- un prick-test ≥ 15 mm correspond 60% de chances pour un TPO positif avec œuf cuit
- le pic en kU/l relevé pour le CAP blanc d’œuf au cours du suivi discrimine mal les futurs tolérants : 32% de tolérants à l’âge de 8 ans pour un pic à 2-5 kU/l, 11% de tolérants pour un pic > 50 kU/l
Un TPO négatif pour l’œuf cuit est aide à réintroduire progressivement l’œuf ![]() . La cuisson doit cependant être suffisante et constante (ex.
. La cuisson doit cependant être suffisante et constante (ex. ![]() ).
).
Œufs et CCD
(voir aussi : Les CCD)
Plusieurs allergènes du blanc d’œuf de poule sont glycosylés ![]()
![]() : l’ovalbumine, l’ovomucoïde, l’ovoinhibiteur, l’ovoglycoprotéine….
: l’ovalbumine, l’ovomucoïde, l’ovoinhibiteur, l’ovoglycoprotéine….
Leurs chaînes glucidiques ne semblent pas participer à l’IgE-réactivité du blanc d’œuf : la déglycosylation de l’ovomucoïde n’altère pas son IgE-réactivité ![]()
![]() .
.
La capture des IgE anti-broméline et anti-HRP n’a pas d’effet sur la réactivité in vitro pour le blanc d’œuf ![]() . Les chaînes glucidiques végétales ne croisent dont pas avec les glycanes des protéines d’œuf.
. Les chaînes glucidiques végétales ne croisent dont pas avec les glycanes des protéines d’œuf.



